
The CARE Course
Critical Procedure - Cardiac pacing
Back to Critical Procedures - Index page
Home
For all procedures, ask yourself, 'does this need to be done 'now vs later'? And should this be done by 'me vs someone else?' Very often the answers will be 'now' and 'me' - so read on!
Cardiac pacing
Description
How to perform cardiac pacing for 'unstable' bradycardias.
Indications
 |
'Unstable' bradycardias (typically HR < 50, and a 3rd degree or 'Mobitz II, 2nd degree block) that have not responded to atropine - or when vascular access is not readily available - see Bradycardia algorithm in the ACLS 2020 guidelines.
If atropine is not effective, then consider dopamine infusion at 2-10 mcg/kg/min or epinephrine infusion at 2-10 mcg/minute or transcutaneous pacing.
In ACLS, 'unstable' is defined as the presence of one or more of
- hypotension
- new altered level of consciousness
- signs of shock
- ischaemic chest pain
- new or worsening cardiac failure
A search for the 5 H's and 5 T's should be made but this should not delay treating the heart rate of the unstable patient who has bradycardia.
Contraindications
None, once the diagnosis of unstable bradycardia is made.
Equipment
Monitor/defibrillator/pacer
IV cannula
Resuscitation equipment
Fentanyl and midazolam
Procedure
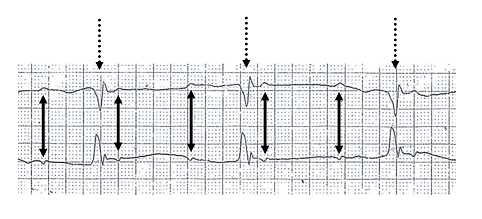
 Electrical capture |
- the pacing/defibrillator pads will probably already be in place, if not, place them on the patients chest, they can be in the standard position or in an antero-posterior configuration with one on the anterior left chest (marked 'Apex' or with a heart icon) and one on the posterior left chest - ensure you have the pads the right way around
- 3 or 4 lead monitoring should also be attached - you will monitor via the leads and pace via the pads
- explain to the patient and team what you propose to do
- sedation and analgesia are advisable if the patient is awake, depending on the urgency of the situation (a small dose of midazolam and fentanyl is usually adequate)
- turn the pacer functionality on and check that the QRS complexes are 'marked' (increase the ECG size and/or switch to another lead if necessary)
- set the demand pacing rate to 70-80 beats per minute
- turn up the current until electrical capture (see image) is seen on the monitor (usually around 60 mAmps but may be higher)
- check that there is a pulse ie. that mechanical capture is achieved
- reduce the current (mAmps) to the lowest level required for capture and then increase the current by 5-10 mAmps to allow for reduction in pad conduction, patient movement etc
Potential pitfalls
Improperly positioned or adhered pacing pads. Poor contact.
Not having the 3 (or 4) lead monitoring on.
Inadequate analgesia/sedation.
Failure to check for mechanical capture / patient improvement.
Failure to maintain monitoring of electrical and mechanical capture.
"Plan B"
Find and treat the cause of the bradycardia.
Chronotropes if not already tried - dopamine or epinephrine (see above).
Trans-venous pacing if available.
