
The CARE Course

Critical Procedure - Synchronised cardioversion
Back to Critical Procedures - Index page
Home
For all procedures, ask yourself, 'does this need to be done 'now vs later'? And should this be done by 'me vs someone else?' Very often the answers will be 'now' and 'me' - so read on!
Synchronised cardioversion
Description
How to perform synchronised cardioversion for 'unstable' tachycardias.
Indications
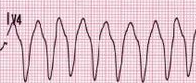 VT |
 SVT |
'Unstable' tachycardias - see ACLS Tachycardia algorithm 2020.
In ACLS, 'unstable' is defined as the presence of one or more of
- hypotension
- new altered level of consciousness
- signs of shock
- ischaemic chest pain
- new or worsening cardiac failure
Contraindications
This procedure is not for pulseless VT or for VF. Both of these should be treated with unsynchronized defibrillation.
Cardioversion of atrial fibrillation requires caution to reduce the risk of embolic stroke from the procedure. The patient should be:
- fully anticoagulated for 3 weeks prior OR
- unstable and in rapid need of rhythm control (thus accepting the higher risk of stroke) OR
- onset within 12 hours OR
- rhythm is AF with onset within 48 hours AND with a CHADS2 risk score of <2
Equipment
Monitor/defibrillator.
IV cannula
Resuscitation equipment
Procedure
 |
 |
 |
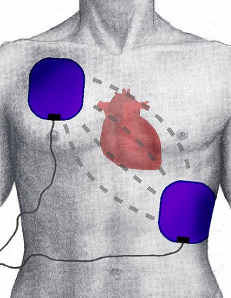
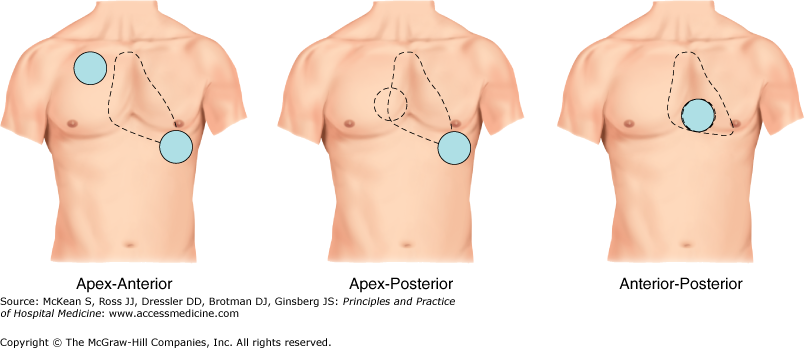
- the defibrillation pads will probably already be in place, if not, place them on the patients chest in the positions indicated on the pads
- if there is time and the patient can comprehend, explain to the patient what you propose to do and get consent
- explain to the team what you are going to do
- sedation is necessary if the patient is awake, depending on the urgency of the situation
- brief sedation with propofol is usually adequate - alternatively midazolam could be used
- evidence suggests no need for adding an opiate (which increases the hypotension and apnoea risk)
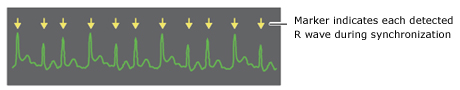
- select 'Sync' on the monitor and ensure it is marking the R waves (this is to avoid delivering a shock on the T wave which can precipitate VF)
- select the energy level.
Initial energy levels in Joules VT (monomorphic) 100 100 AF 120-200 200 Atrial flutter / SVT 50-100 50-100 VT (polymorphic eg. Torsades) Unsyncrhonized 200 Unsyncrhonized 200 - ensure everyone is clear, before briefly re-checking the monitor and pressing and holding the Shock button. Say 'you're clear, I'm clear, still in (whichever rhythm), shocking....'
- you may need to hold the 'Shock' button for a brief time to allow the defibrillator to deliver the shock at the correct, synchronised time
- if tachycardia persists, increase the energy by perhaps 50 J or more, re-select Sync, and repeat the process
Potential pitfalls
Improperly positioned or adhered defibrillation pads.
Inadequate safety when delivering a shock.
Not checking that the defib is 'synched' every shock.
Not holding the Shock button long enough for a shock to be delivered.
"Plan B"
Synchronised cardioversion is usually successful.
In case of failure, review pharmacological options and/or attempt to discuss with a cardiologist.